Migraine Specialist Gilbert AZ
Basics of Migraine Headaches
Migraine headaches are a common problem affecting 36 million Americans, about 12% of the population. They are severe, painful headaches that may begin with sensory warning signs such as flashes of light, tingling of arms and legs, and blind spots. Vomiting, nausea, and increased sensitivity to light and sound are other symptoms. The pain of a migraine can be excruciating and last for hours to days.
begin with sensory warning signs such as flashes of light, tingling of arms and legs, and blind spots. Vomiting, nausea, and increased sensitivity to light and sound are other symptoms. The pain of a migraine can be excruciating and last for hours to days.
The exact cause of migraine headaches is unknown; it is thought to be due to abnormal brain activity causing a temporary alteration in the nerve signals, blood flow, and chemicals in the brain. The headaches can be very debilitating and affect women more often than men.
Facts and Statistics
A few facts about migraines are:
- Many times, a migraine sufferer can prevent a full-blown attack by recognizing and acting upon the warning signs.
- Reduce or eliminate pain with over-the-counter medications.
- Preventive medication can be taken by people who suffer from severe attacks.
- Approximately 12% of Americans get migraine headaches.
- The age for most migraine sufferers is usually between 15-55 years of age.
- Light, stress and many times allergies may trigger migraines and can be identified by the sufferer as a cause prior to the headache.
- A warning prodrome, preceding the onset of a migraine headache, can be noticed at times.
- Migraine cause is still unknown.
- An aura of sensory disturbances, followed by a severe one-sided headache, is noticed many times before the migraine.
Causes and Triggers
As mentioned, many migraine sufferers may be able to identify triggers that cause the headaches. A few migraine headache triggers are:
- Bright or flickering lights
- Loud noises
- Temperature changes
- Smoky or strong smells (detergents, perfumes, air fresheners, and more)
- Allergies
- Sleep disturbances or irregular sleep
- Emotional or physical stress such as anxiety, depression, tension, and excitement
- Tiredness or exercise
- Dehydration
- Smoking
- Skipping meals (low blood sugar)
- Certain foods, such as, tyramine (red wine, smoked fish, aged cheese, figs, chicken livers, certain beans. Also, monosodium glutamate (MSG), nitrates which are in lunch meats, hotdogs, and bacon. Others foods that cause headache include chocolate, nuts, onions, citrus, avocado, peanut butter, bananas, pickled foods, and dairy.
- Alcohol
- Tension headaches
- Birth control pills, sleeping pills, hormone replacement, menopause, or menstrual cycle fluctuations.
Symptoms and Signs
Although not all migraines are the same, typical symptoms and signs include:
- Being physically sick.
- The pain is usually a throbbing, severe, and pulsing pain.
- Physical activity that increases pain.
- Activities can’t be performed due to pain.
- Usually confined to one side of the head during an attack, but can occur on either side of the head and can be moderate to severe.
- Increased sensitivity to light and sound.
- Lying quietly in a darkened room relieves some symptoms.
- Stomach pain, sweating, temperature changes, and diarrhea.
Diagnosis and Treatment
If you are having frequent headaches, and suspect migraine, keep a diary of symptoms, noting the time of onset, any triggers, how long the headache  lasted, any preceding factors or aura, and any other symptoms. This is done to give to your doctor so he/she can determine the headache type and possible cause. A period of six to eight weeks should suffice in recording migraine events.
lasted, any preceding factors or aura, and any other symptoms. This is done to give to your doctor so he/she can determine the headache type and possible cause. A period of six to eight weeks should suffice in recording migraine events.
Migraines are difficult to diagnose due to no specific test can diagnose migraines, even though some tests are used to help diagnose other kinds of headaches. This particular method (called the 5,4,3,2,1 criteria) is used for migraines without an aura:
- 5 or more attacks.
- 4 hours to 3 days-time period.
- At least 2 isolated to one side, moderate to severe pain, aggravation by or avoidance of routine physical activity, and a pulsating feel.
- At least 1 other symptom, such as nausea, vomiting, sensitivity to sound, or sensitivity to light.
Currently there is no cure for migraine headaches. Doctors concentrate on preventing full-blown migraines from happening and try helping rid of symptoms if they come on. Treatments vary from person to person, and these options include rest, getting sleep, avoiding triggers, and lying quietly in a darkened room.
Medications
- Antimetics: Metoclopramide may also be used to control symptoms such as nausea and vomiting.
- Serotonin agonists: If migraines aren’t responding to over-the-counter medications, Sumatriptan may be prescribed for severe migraines.
- Analgesia: The first abortive therapies to eliminate the headache or substantially reduce pain are usually, over-the-counter medications such as
 naproxen, ibuprofen, acetaminophen (paracetamol), and other analgesics like Excedrin.
naproxen, ibuprofen, acetaminophen (paracetamol), and other analgesics like Excedrin. - Antidepressants: Tricyclic antidepressants are prescribed to reduce migraine symptoms although they are not approved in all countries for this particular purpose.
- Ergots: Usually effective if administered at the first sign of a migraine, this is an abortive treatment.
- Painkillers: Should be taken right away before headache lingers.
Interventional Procedures
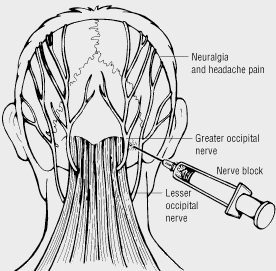
- Occipital Blocks – these have been shown to help decrease the frequency of migraines and work well over 60% of the time.
- Radiofrequency Ablation of the occipital nerves – these are a fairly new treatment, and are showing excellent promise for treating migraines and providing longer relief than the blocks.
- Electrical stimulation – This treatment is minimally invasive and basically helps to mask pain. This treatment is also fairly new and has been showing exceptional outcomes for helping decrease the frequency of migraines.
Dr. Ajay Yeddu is the Gilbert pain management physician at Desert Interventional Spine Consultants. He is a migraine specialist and helps patients routinely achieve relief and get their lives back on track. Most insurance is accepted, call us today!
Resources
Jensen R & Stovner LJ (2008). Epidemiology and comorbidity of headache. The Lancet, 7(4), 354-361.



